All Categories
Featured
Table of Contents
The Best Reproductive Clinic Near Me Albuquerque Nm?
Lots of people need fertility assistance. This consists of males and females with infertility, lots of LGBTQ people, and single individuals who want to raise kids. An approximated 10% of ladies report that they or their partners have ever received medical help to conceive. Despite a requirement for fertility services, fertility care in the U.S.
Typically, fertility services are not covered by public or personal insurers. Fifteen states require some personal insurers to cover some fertility treatment, but substantial spaces in coverage remain. Just one state Medicaid program covers any fertility treatment, and no Medicaid program covers artificial insemination or in-vitro fertilization.

This implies that in the lack of insurance protection, fertility care is out of grab many individuals. Less Black and Hispanic ladies report ever having used medical services to conceive than White ladies. This is a result of numerous aspects, consisting of lower incomes on average among Black and Hispanic females in addition to barriers and mistaken beliefs that may deter women from seeking assistance with fertility.
What Is The Best Fertility Reproductive Center Albuquerque Nm App?
Transgender people undergoing gender-affirming care might also not fulfill requirements for "iatrogenic infertility" that would qualify them for covered fertility conservation. Lots of people need fertility assistance to have kids. This could either be due to a medical diagnosis of infertility, or since they are in a same-sex relationship or single and desire children.
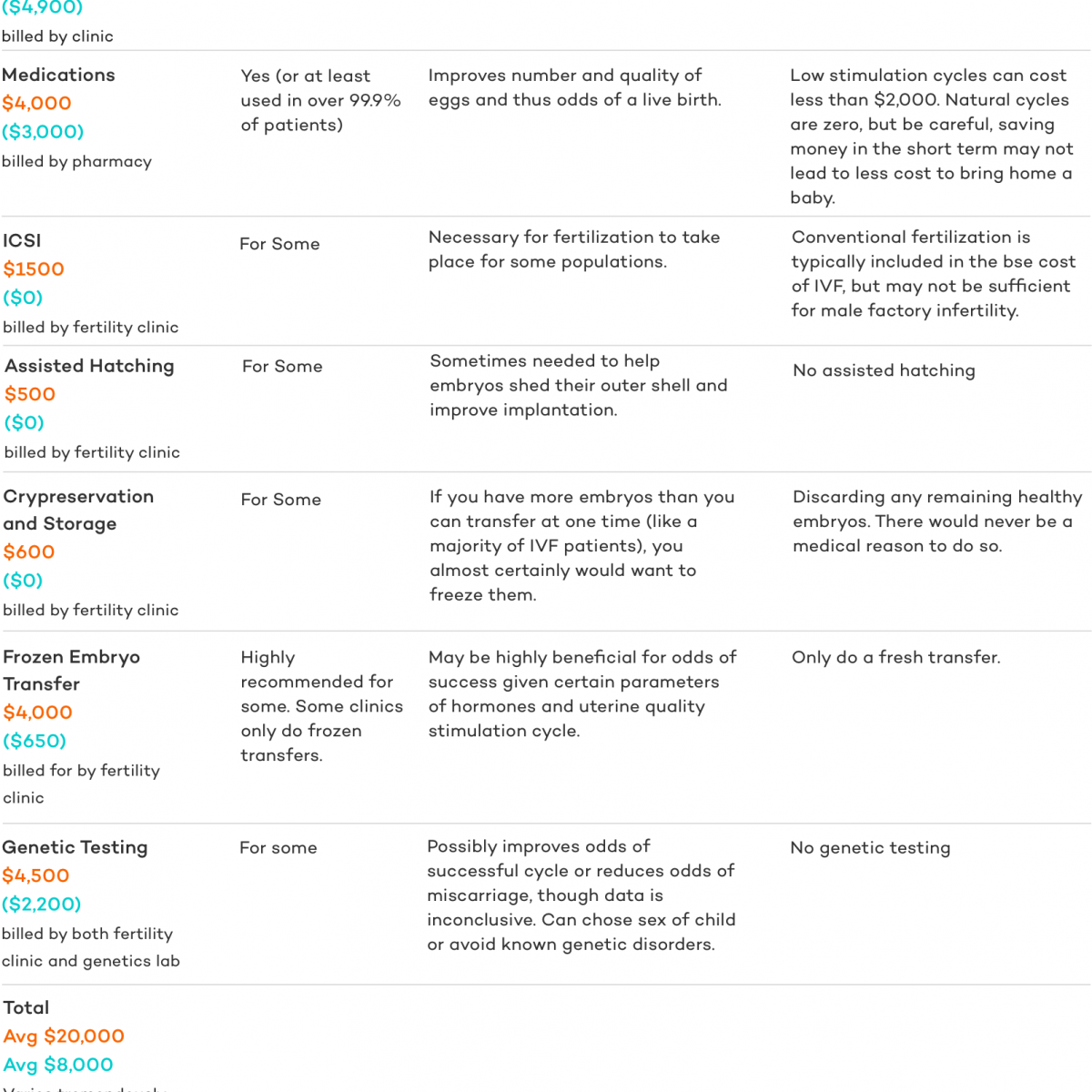
Fertility treatments are pricey and typically are not covered by insurance. While some private insurance strategies cover diagnostic services, there is very little protection for treatment services such as IUI and IVF, which are more pricey. Many people who utilize fertility services need to pay of pocket, with expenses frequently reaching countless dollars.
About 25% of the time, infertility is triggered by more than one factor, and in about 10% of cases infertility is unusual. Infertility estimates, however do not represent LGBTQ or single people who may likewise require fertility support for family structure. For that reason, there are diverse reasons that may prompt people to look for fertility care. rental dumpster.
What Is The Best Infertility Center New Mexico?
Patient Information Series. 2017 Our analysis of the 2015-2017 National Survey of Family Development (NSFG) discovers that 10% of females ages 18-49 say they or their partner have ever talked with a physician about methods to assist them end up being pregnant (information not shown).3 Among ladies ages 18-49, the most typically reported service is fertility suggestions ().
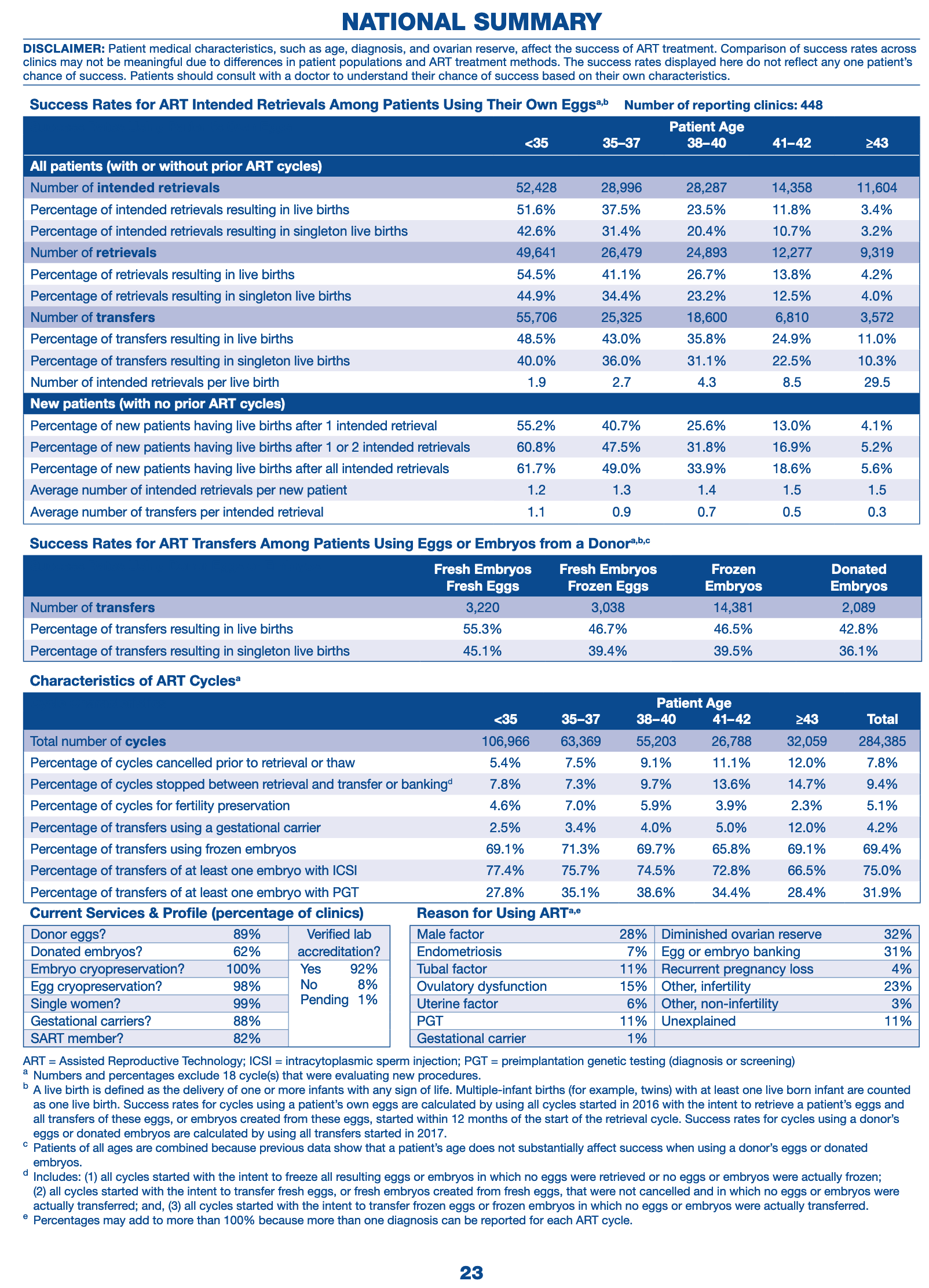
Many clients do not have access to fertility services, largely due to its high cost and limited coverage by personal insurance coverage and Medicaid. As an outcome, many individuals who use fertility services should pay of pocket, even if they are otherwise insured. Out of pocket costs vary extensively depending on the client, state of house, service provider and insurance plan (dumpster rental cost).
Figure 3: Fertility Treatments Usually Expense Clients Countless Dollars Insurance protection of fertility services differs by the state in which the person lives and, for individuals with employer-sponsored insurance coverage, the size of their employer. Lots of fertility treatments are ruled out "medically essential" by insurance provider, so they are not usually covered by private insurance strategies or Medicaid programs.
What Is Full Service Ivf Doctor Albuquerque Nm?
g., screening) are most likely to be covered than others (e. g., IVF). A handful of states need coverage of fertility services for some fully-insured private plans, which are managed by the state. These requirements, however, do not use to health strategies that are administered and funded directly by employers (self-funded strategies) which cover six in ten (61%) workers with employer-sponsored medical insurance.
Two states (CA and TX7) need group health plans to provide at least one policy with infertility coverage (a "required to provide"), but employers are not required to select these strategies. Figure 4: The Majority Of States Do Not Require Private Insurers to Provide Infertility Benefits Nevertheless, in states with "mandate to cover" laws, these just use to specific insurance companies, for specific treatment services and for particular clients, and in some states have monetary caps on expenses they must cover ().
In other states, nearly all insurers and HMOs are included in the required (Dumpsters Plymouth MA). Lots of states provide exemptions for small employers (
Latest Posts
Who Is The Best Ivf Clinics Near Me New Mexico Company?
Which Is The Best Ivf Fertility Clinic New Mexico Plan
What's The Best Ivf Doctor Albuquerque Nm Brand